 X-rays are a type of ionizing radiation. Radiation is considered ionizing when the energy is high enough to produce ions by breaking molecular bonds and displacing (or removing) electrons from atoms or molecules. Ionizing radiation has a number of beneficial uses that include cancer treatment, medical equipment sterilization, and scientific research. However, unsafe use of ionizing radiation is potentially harmful and can result in permanent effects on DNA, severe skin or tissue damage, and cancer.
X-rays are a type of ionizing radiation. Radiation is considered ionizing when the energy is high enough to produce ions by breaking molecular bonds and displacing (or removing) electrons from atoms or molecules. Ionizing radiation has a number of beneficial uses that include cancer treatment, medical equipment sterilization, and scientific research. However, unsafe use of ionizing radiation is potentially harmful and can result in permanent effects on DNA, severe skin or tissue damage, and cancer.
The X-Ray Safety Manual contains procedural guidelines and information for prudent work practices while using any x-ray producing device (XPD) at USC. The manual is made available to every area authorized to use XPDs and any area where XPDs are present.
How do I:
- Get approval to purchase an XPD?
- Register, transfer, or dispose of an XPD?
- Email radsafety@usc.edu to begin the process. XPDs must be registered within thirty (30) days of the acquisition date.
- What needs to be registered?
- Obtain a dosimeter badge and ring?
Safety Tips and Guidelines
Additional safety tips and guidelines are available for the following x-ray equipment and techniques.
- Cabinet X-Ray
- Electron Microscope
- Handheld Dental X-ray Unit
- Handheld X-ray Fluorescence Analyzer
- Veterinary Research Fluoroscopy
- X-ray Diffraction
Resources
- X-Ray Safety Manual
- X-Ray Safety and Emergency Procedures – fillable form
Cabinet X-Ray
A cabinet X-ray device is an entirely shielded system that stops most radiation from leaving the enclosure. Examples of cabinet X-ray systems at USC include X-ray irradiators and digital X-ray cabinets.
The enclosure is typically made of lead and is designed to attenuate radiation to levels below 0.5 mR/hr at any point 5 centimeters from any surface of the device. Lead PPE and personal dosimetry are not required when using a cabinet X-ray device because radiation remains at background levels during operation.
Device Users are advised to continue following ALARA (as low as reasonably achievable) principles when using the device:
- Time: Minimize your time around the energized device.
- Distance: Maximize your distance away from the device. Do not stand too close to the machine during operation.
- Shielding: Do not tamper with the shielding built into the device.
Cabinet X-ray devices have safety features that prevent X-ray production when the X-ray source is accessible and warn the user when X-rays are being produced. Examples of interlocks include:
- A physical interlock in the door that breaks the circuit controlling X-ray production when the door is opened
- An electrical sensor that stops X-ray production when the door is opened
- Lights indicating when X-rays are being produced or when the shutter is open
- An alarm indicating that the shutter is open
It is essential to maintain the integrity of the shielding and safety devices by following these safe practices:
- Do not bypass any safety interlocks.
- Do not tamper or alter the device shielding.
- Do not attempt to repair the device. Contact the manufacturer.
- Use the device only for its authorized use.
- Complete preventative maintenance, as recommended by the device manufacturer.
The Radiation Safety Office will complete a leakage survey upon installation or any major repair and constantly monitors all rooms that house a cabinet X-ray device for leakage radiation with area dosimeters. All device malfunctions or suspected incidents must be reported to the Radiation Safety Officer immediately.
Reference
Title 17 California Code of Regulations Subchapter 4. Radiation
Electron Microscope
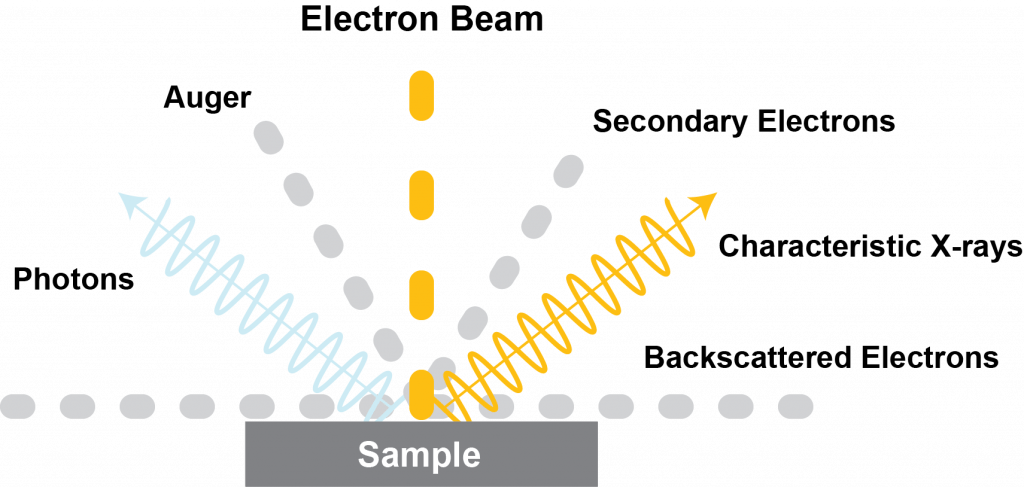 Electron microscopes (EM) produce low levels of X-rays as a result of the electron beam interacting with the sample material. Modern EMs are well-shielded; they eliminate or greatly minimize exposure to personnel. Personal dosimetry is not required when working with an EM.
Electron microscopes (EM) produce low levels of X-rays as a result of the electron beam interacting with the sample material. Modern EMs are well-shielded; they eliminate or greatly minimize exposure to personnel. Personal dosimetry is not required when working with an EM.
To ensure exposures are As Low As Resonably Achievable (ALARA), EM users will conduct the following:
- Ensure that shielding, safety interlocks, and warning lights are maintained and operable.
- Turn off EMs when not in use.
- Reduce time around energized EMs.
- Maximize distance away from energized EMs. Keep hands/arms off the energized EM unless working with it.
Additionally, EM users must:
- Know safe operating and emergency procedures.
- Complete device-specific training with the Supervisor of the EM.
- Never alter the original design or shielding of the EM without written approval from the Radiation Safety Officer (RSO).
- Log user name and date of EM usage.
- Notify the EM Owner/Supervisor and RSO of any radiation incidents or unsafe practices.
EM Owners/Supervisors must:
- Document all training given to EM Users.
- Notify the RSO of the installation, relocation, disposal, or
transfer of the EM. - Provide written operating and emergency procedures to EM Users.
- Secure the EM from unauthorized users.
- Email radsafety@usc.edu to begin registration of the EM. NOTE: All EMs (e.g., transmission, scanning, reflection, scanning transmission, low voltage) must be registered with the California Department of Public Health (CDPH) and USC Radiation Safety within thirty (30) days of acquisition.
Download the Electron Microscope Safety Guide Sheet to review and record user compliance.
Handheld Dental X-ray Unit
Individuals who operate dental X-ray units must be aware of the risks of radiation and follow safe work practices to keep patient exposure and their own exposure As Low As Reasonably Achievable (ALARA).
Operator Safety
Handheld X-ray units have a backscatter shield installed to protect the operator from backscattered radiation. The location of the shield and positioning of the patient is essential to maximize the shielded area (green) from backscatter radiation (red) – see illustrations. The operator should remain in the shielded area during the exposure.
Patient Safety
-
- Exposure time increases when the imaging angle varies from 90 degrees (or perpendicular) to the film or sensor. Adjust the patient’s head as needed to maintain proper perpendicular alignment.
- Always use the lowest exposure settings possible that provide an image of diagnostic quality.
- Use lead protective aprons and thyroid collar whenever possible. The thyroid gland is especially radiosensitive in children.
- Limit the number of images to a minimum necessary to obtain essential diagnostic information. Carefully plan each exposure to prevent the need for repetition.

References
Aribex- Nomad Pro 2 Operator Manual
California Dental Association- Radiation Safety in Dental Practice
American Dental Association (ADA) and Food and Drug Administration (FDA)
Handheld X-ray Fluorescence Analyzer
These guidelines do not apply to handheld dental units. For more information, see Handheld Dental X-ray Unit above.
X-ray fluorescence is the emission of characteristic X-rays from excited atoms in a material that was bombarded with X-rays. X-ray Fluorescence Analyzers (XFAs) use this phenomenon for non-destructive elemental and chemical analysis and are typically used for research in geochemistry and archaeology.
Primary Beam Risks
When operated at its maximum voltage setting, a typical XFA can deliver a dose of more than 4,000 rads in one hour. Acute effects of radiation exposure to the skin can be found in Table 1. The operator must keep all body parts as far away from the nose of the device (where the beam shutter is located) as possible.
Scatter Radiation Risks
Some radiation is scattered back toward the operator and is dependent on the density of the sample material. Scatter radiation is monitored by Radiation Safety by placing a dosimeter on the device at the typical location of the operator’s hand. Although scatter radiation is less of a hazard than the primary beam, the operator must keep his/her hands and eyes away from the nose of the device at all times.
Safety Features
- An infrared sensor at the nose of the device prevents the unit from emitting X-rays in the absence of a sample in front of it. Note: This does not stop the device from emitting X-rays if a body part is in front of the device.
- Warning lights illuminate when X-rays are being generated.
Proper Setup
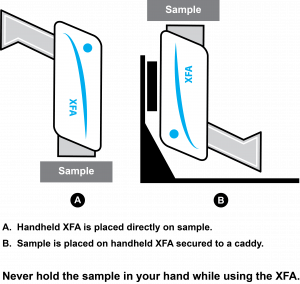 Do not hold the sample to the window of the device by hand. Instead, bring the window of the device to the sample. If the object cannot stand on its own, place the sample down on a surface, or use a benchtop stand (see Figure 1).
Do not hold the sample to the window of the device by hand. Instead, bring the window of the device to the sample. If the object cannot stand on its own, place the sample down on a surface, or use a benchtop stand (see Figure 1).- Be aware of the direction of the direction that the X-rays travel. XFAs typically emit X-rays at an upward angle.
- The device should always be pointed away from any other people or the general public. Anyone not operating the device should stay at least 3 feet away.
- When working in a lab, designate an area for sample analysis. The XFA should point toward an unoccupied area of at least a 3 foot radius. Do not assume that a wall or partition provides safe shielding for people on the other side. If using the device near a wall or barrier, ensure no one is on the other side.
- When working in the field, clear the area before beginning analysis and verbally notify anyone working around you. Use indicators (e.g. cones, barriers) to prevent others from entering the area.
- Use a benchtop stand if low-density samples are measured frequently. More radiation is backscattered and less radiation is attenuated when analyzing low density samples (e.g. plastic, wood, soil), which can cause a higher dose to the operator.
Table 1. Responses of the Skin to Radiation
| Response | Description | Time of Onset | Threshold (rads) |
|---|---|---|---|
| Early transient erythema | Inflammation of the skin | Within hours | 200 |
| Epilation | Hair loss | 14-21 days | 300 |
| Main erythema | Inflammation of skin | Days to weeks | 300 |
| Dry desquamation | Atypical keratinization of the skin | 3-6 weeks | 800 |
| Dermal atrophy | Thinning of the dermal tissues | > 26 weeks | 1000 |
| Moist desquamation | Loss of the epidermis | 4-6 weeks | 1500 |
| Secondary ulceration | Secondary damage to the dermis | > 6 weeks | 1500 |
| Acute ulceration | Early loss of the epidermis | < 14 days | 2000 |
| Late erythema | Inflammation of the skin | 8-20 weeks | 2000 |
| Dermal necrosis | Necrosis of the dermal tissues | > 10 weeks | 2000 |
| Invasive fibrosis | Healing method that leads to scar tissue formation | Months to years | 2000 |
| Telangiectasia | Atypical dilation of the superficial dermal capillaries | > 52 weeks | 4000 |
| Acute epidermal necrosis | Interphase death of postmitotic keratinocytes in the upper visible layers of the epidermis | < 10 days | 55,000 |
References
CDC – Cutaneous Radiation Injury (CRI): A Fact Sheet for Clinicians
Bruker AXS Handheld, Inc. X-ray Radiation Safety Operator Training Manual
Centers for Disease Control and Prevention (CDC)
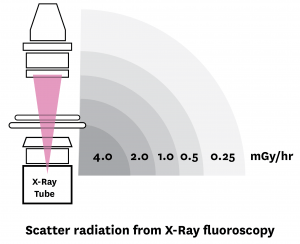
Veterinary Research Fluoroscopy
Fluoroscopy is a method of continuous X-ray imaging that allows for real-time monitoring of a procedure. The primary fluoroscopy beam produces radiation at a rate of 2000-5000 mR/minute and produces high levels of scatter radiation when the animal on the table is exposed to it.
 In order to keep exposure to personnel as low as reasonably achievable (ALARA), the following principles must be followed:
In order to keep exposure to personnel as low as reasonably achievable (ALARA), the following principles must be followed:
- Time. Minimize the time that the device is on. Complex interventional procedures (e.g., placing devices inside of the body) require fluoroscopy to be administered for long periods of time. Work efficiently and only image when required.
- Distance. Personnel working closest to the animal (e.g., the surgeon or injector) must maximize the distance between:
- Their hands and the primary beam
- Themselves and the table without being uncomfortable
- All other essential personnel must stay as far away from the unit as possible. All non-essential personnel must not be in the room while imaging is in progress.
- Shielding. Any personnel in the room during imaging must wear protective equipment and use shields as necessary.
Personnel must:
- Avoid the primary X-ray beam.
- Wear protective equipment (e.g., lead aprons and thyroid collar, leaded goggles, leaded gloves).
- Use shielding (e.g., mobile shields, lead curtains), when possible.
- Be aware of the position of the beam.
- Know how to position themselves and the machine for the minimum dose.
References
Operator Shielding: How and Why
Medical X-ray Imaging, FDA
X-ray Diffraction
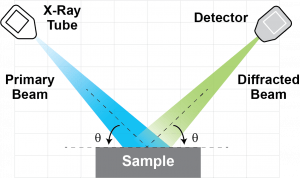 X-ray Diffractometers (XRDs) determine the molecular structure of crystalline materials by analyzing the interference patterns of diffracted X-rays. The primary beam is typically made up of a large amount of low energy X-rays. Typical XRDs can produce a primary beam that delivers thousands of rads in one minute. These X-rays are easily shielded with protective housing, but even a short exposure (less than one second) to the primary beam can cause significant damage.
X-ray Diffractometers (XRDs) determine the molecular structure of crystalline materials by analyzing the interference patterns of diffracted X-rays. The primary beam is typically made up of a large amount of low energy X-rays. Typical XRDs can produce a primary beam that delivers thousands of rads in one minute. These X-rays are easily shielded with protective housing, but even a short exposure (less than one second) to the primary beam can cause significant damage.
Low energy X-rays are readily absorbed in the first few millimeters of the skin. The primary beam is collimated to a small beam diameter, which increases the risk of a severe, localized injury. Acute effects of radiation exposure to the skin can be found in Table 1.
Examples of Warning Displays
- Warning lights indicating that X-rays are being generated
- Warning lights indicating that the X-ray window (i.e. shutter) is open
- Warning lights indicating that the protective housing doors are open.
- Alarm sounding when protective housing doors are opened.
DO NOT
- Do Not bypass elements of the radiation protective housing, safety switches of the panel elements, or built-in interlocks.
- Do Not handle, manipulate, or adjust any object in the direct beam path (e.g. sample, sample holder, collimator) while the beam is on.
- Do Not attempt to repair or modify the unit.
DO
- Receive device-specific training on the unit’s safe operation from the Device Supervisor responsible for the unit. All Device Users must also have Radiation Safety Training.
- Verify that warning displays, interlocks, and protective housings are intact and functioning prior to operating the unit.
- Keep up with routine preventative maintenance to prevent device failure.
- Follow all safety protocols and SOPs specific to the unit in your lab.
- Report any malfunctions or unusual occurrences to the Device Supervisor and the Radiation Safety Office.